Small eyes make cataract surgery more difficult in many ways: there is less working room in the eye, the IOL calculations are less accurate, and our standard incision has more of an astigmatic effect. But these are among our happiest patients because we are able to treat large degrees of hyperopia and give patients a near plano outcome and excellent vision without glasses.
Pre-op Evaluation
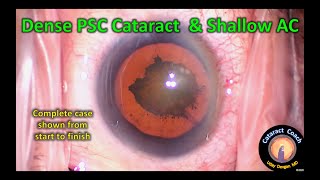
Small eyes have a shorter axial length, typically less than 22 mm (often closer to 20 mm), and accompanying hyperopia of +3 D or more. The anterior chamber can be shallow, with measured depths of 2 mm or less and associated narrow angles. In cases where there are advanced cataractous changes, the lens can swell and further narrow the angles.
The cornea should be carefully evaluated for endothelial weakness because there is a higher chance of phaco-induced cell loss due to the closer proximity of the phaco probe. Small corneal size can also mean that the standard-size phaco incision may induce more astigmatic change at the time of cataract surgery.
When measuring the axial length, small errors can result in more of a refractive shift than in normal or large eyes. Whereas an axial length that is wrong by 1 mm in a normal eye may induce 3 D of error, in a short eye this can be increased to 4 D or even 5 D. Difficulty predicting the final effective lens position of the IOL also means that the lens calculations are more like estimations.
IOL Calculations
Certain formulae have been shown to be more accurate in these short eyes. Of the older two-variable formulae, the Hoffer Q tends to do better in the setting of axial lengths less than 22 mm. However, it is advisable to use newer formulae like the Ladas Super Formula, Haigis, Barrett, and Holladay 2, which incorporate additional data such as anterior chamber depth, to produce more accurate results.
Single-piece acrylic IOLs, as well as three-piece acrylic and silicone IOLs, are appropriate choices because they all have flexible haptics that allow placement within the smaller-than-usual capsular bag. In some situations, eyes with very short axial lengths may need an IOL power that is particularly high, such as +30 D, +35 D or even more. Because different IOL designs come in different ranges, every effort should be made to source the appropriate lens. In the United States, there is at least one single-piece acrylic IOL (AcrySof SA60AT) available in powers up to +40 D.
It is better to have a single IOL with the correct power than to piggyback using two IOLs to achieve the same dioptric strength.
In the rare eyes in which a power of more than +40 D is indicated, it may be advisable to do the surgery in two stages: cataract surgery with implantation of the maximum power IOL (+40 D) in the capsular bag, followed by a second surgery with implantation of a piggyback lens in the ciliary sulcus if there is sufficient room. This provides more refractive accuracy because the power of the second IOL, which is placed in the sulcus, is determined based on the postoperative refraction after the initial cataract surgery.
Surgical Technique
There are certain risks, such as choroidal hemorrhage, that are more common in these smaller eyes. In addition, the shallow anterior chamber can make it more difficult to complete the capsulorrhexis and atraumatically remove the nucleus. After creation of an initial paracentesis, the anterior chamber can be inflated with a cohesive viscoelastic to create space and deepen the anterior chamber.
The corneal endothelium should then be protected with a dispersive viscoelastic. Because the volume of the anterior chamber is less, there is a limited amount of working room during phacoemulsification. The closer the phaco probe is to the cornea, the greater the potential for endothelial damage. For this reason, phaco techniques performed within the capsular bag are preferred over supra-capsular methods. Once the cataract is removed and the new IOL is inserted in the capsular bag, care should be taken to ensure that the incisions are watertight. Because these small eyes often have smaller corneas, the standard-sized phaco incisions may encompass a larger area and arc length and may not seal as well.
Post-Op Follow-Up
These patients tend to be particularly happy in the postoperative period because their high degree of hyperopia has been corrected. But there are additional benefits, such as restoration of the angle anatomy and lowering of the IOP, which occurs because the 4-mm thick cataract has been replaced by a 1-mm thin IOL. With careful preoperative planning and appropriate intra-operative techniques, we can successfully perform cataract surgery on these small eyes.









Информация по комментариям в разработке