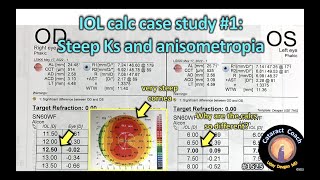
use the refractive results of the first cataract surgery to hone the IOL calcs of the other eye
Скачать use the refractive results of the first cataract surgery to hone the IOL calcs of the other eye бесплатно в качестве 4к (2к / 1080p)
У нас вы можете скачать бесплатно use the refractive results of the first cataract surgery to hone the IOL calcs of the other eye или посмотреть видео с ютуба в максимальном доступном качестве.
Для скачивания выберите вариант из формы ниже:
Cкачать музыку use the refractive results of the first cataract surgery to hone the IOL calcs of the other eye бесплатно в формате MP3:
Если иконки загрузки не отобразились, ПОЖАЛУЙСТА,
НАЖМИТЕ ЗДЕСЬ или обновите страницу
Если у вас возникли трудности с загрузкой, пожалуйста, свяжитесь с нами по контактам, указанным
в нижней части страницы.
Спасибо за использование сервиса video2dn.com








Информация по комментариям в разработке